
MIU faculty propose innovative “unifying systems medicine approach” to address physician burnout epidemic
The journal Heart and Mind, a respected peer-reviewed medical journal, recently published an editorial by three MIU faculty describing a holistic “unifying systems medicine model” that encompasses and unites all aspects of health — mind, body, environment, and consciousness.
They focus their approach on addressing the epidemic of physician burnout and holistically improving physicians’ mental health and well-being.
The article is being picked up in the media — for example, Science Magazine, the Global Neurology Academy, the Global Women’s Health Academy, Medtelligence, reachmd/com, and more.
Physician burnout has become an epidemic in the US and around the world. More than 50% of physicians and healthcare providers report symptoms of burnout. Burnout impairs physicians’ quality of life, increases their risk of cardiovascular disease and mental health disorders, and impedes their ability to care for their patients. Physician burnout costs the US an estimated $4.6 billion annually.

“Healthcare provider burnout is a major threat to health care quality, patient outcomes, and the medical workforce,” said Robert Schneider, MD, FACC, Dean of the MIU College of Integrative Medicine, and senior author of the paper. “Urgent action is required to alleviate this crisis.”
The new model incorporates biological, psychological, environmental, and consciousness factors into an interconnected framework the authors call the Connectome of Health. The model emphasizes the role of the Transcendental Meditation technique in enhancing resilience and preventing burnout and related mind-body conditions such as cardiovascular disease.
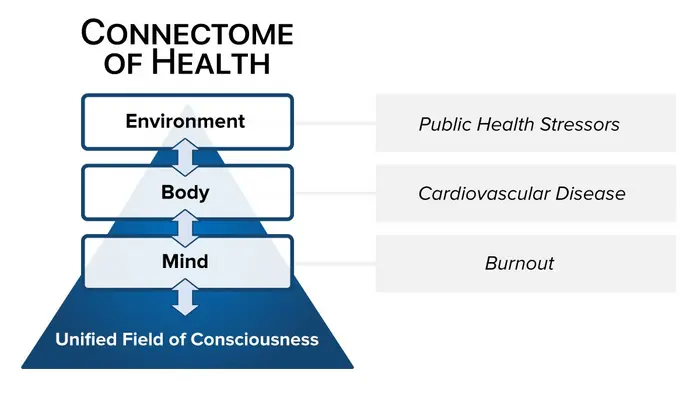
The diagram above illustrates how the proposed systems medicine model incorporates four fundamental domains of health: environmental health (environment), physical health (body), mental health (mind), and spiritual health (unified field of consciousness).
“The spiritual domain corresponds to the unified field of quantum physics,” Schneider said. “In the Connectome model, the unified field is identified as a field of consciousness that underpins both mind and matter. As such, we term it the unified field of consciousness. Each of these four domains interacts with the others, forming an interconnected whole system — The Connectome of Health.”
“Transcendental Meditation allows the mind to experience a unique state of restful alertness, providing a buffer against the stresses of medical practice,” explained Fred Travis, PhD, co-author and director of the MIU Center for Brain, Consciousness, and Cognition.
The authors reviewed studies showing that TM practice reduces symptoms of burnout, anxiety, depression, and PTSD in healthcare providers. One of the largest studies on the effects of TM practice in a healthcare setting was conducted at three Miami hospitals during the height of the Covid crisis, where the effects were almost immediate.
“After two weeks, symptoms of depression and anxiety decreased nearly 45%, while insomnia, emotional exhaustion, and well-being improved significantly. These changes became even more significant throughout the three-month study,” reported Mark Nestor, MD, PhD, lead investigator and Voluntary Professor at the University of Miami Miller School of Medicine.
The Heart and Mind authors suggest that TM’s benefits stem from unique neural mechanisms that counter the brain patterns underlying burnout and simultaneously balance interconnections between body, mind, environment and consciousness.

“This systems approach highlights the value of developing consciousness through meditation for cultivating mental, physical and social health in an integrative manner,” said Tony Nader, MD, PhD, co-author, and Director of the Dr. Tony Nader Institute at MIU. “It offers a new paradigm for preventing disease and promoting whole health.”
The researchers call for continued investigation and application of this framework to tackle burnout and transform healthcare. “By incorporating evidence-based meditation programs, we can create a new wellness model that supports clinicians’ health and improves care for all,” Schneider said.
“Physician burnout is an on-going predicament that gained prominence with Covid-19,” said Marie Loiselle, PhD, director of evaluation and assessment at MIU, who did her doctoral research on the effects of Transcendental Meditation practice on academic physician burnout and depression (see below). “This editorial by Schneider, Travis, and Nader not only updates our understanding of the impact and scope of the problem, but perhaps more importantly presents empirical solutions to it. Specifically, they explain how the TM technique works in diminishing burnout on the neuro and cardiovascular levels.”
In 2021 the American Heart Association published a statement acknowledging the lack of a holistic approach. “As clinicians delivering health care, we are very good at treating disease but often not as good at treating the person,” the statement said. “The focus of our attention has been on the specific physical condition rather than the patient as a whole. Less attention has been given to psychological health and how that can contribute to physical health and disease.” The statement went on to acknowledge the “increasing appreciation of how psychological health can contribute not only in a negative way to cardiovascular disease (CVD) but also in a positive way to better cardiovascular health and reduced cardiovascular risk.”
Although the AHA statement acknowledged the role of mind along with body, mind and body comprise only two of the four elements in the holistic Connectome of Health model.
Further resources
“Effects of Transcendental Meditation on Academic Physician Burnout and Depression: A Mixed Methods Randomized Controlled Trial,” article in the Journal of Continuing Education in the Health Professions. 43(3):143-144, Summer 2023, by Marie Loiselle*, Carla Brown, Frederick Travis*, Gregory Gruener, Maxwell Rainforth*, and Sanford Nidich*. *Denotes MIU faculty.
NEW — Podcast interview with three authors of the above study (Loiselle, Brown, and Gruener), October 17, 2023.
Thank you to Dr. Robert Schneider for his contributions to this story.
